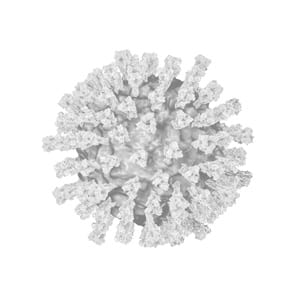
2006 Rotavirus
Rotaviruses are the most common cause of severe diarrheal disease and leading cause of gastroenteritis in young children worldwide. Prior to the introduction of the first attenuated live viral vaccines in 2006, each year more than 400,000 young children were seen by their physician for illness caused by rotavirus, with over 200,000 ER visits and 55–70,000 resulting hospitalizations in the U.S. Globally, rotavirus kills about 450,000 children under the age of 5 each year, with many of these deaths occurring in developing countries. Since recommended routine infant immunization in 2006, the CDC reports hospitalization rates for acute gastroenteritis dropped by 45% in 2008 compared to pre-vaccination (2000–2006), and it is estimated that the rotavirus vaccine prevented 55,000 hospitalizations in 2008. In Mexico, one of the first countries to receive the rotavirus vaccine in 2006, there was a reported 30% reduction in deaths from diarrheal disease in children ages 1–2 years old, and a 40% reduction in children younger than 11 months.6